
Bulbous Nose Rhinoplasty: Techniques Surgeons Use to Refine the Nasal Tip
A bulbous nasal tip is one of the most frequent concerns among rhinoplasty patients—and one of the most misunderstood. Unlike […]
Hair transplantation is often viewed as a golden ticket to restoring a full head of hair. But the truth is […]
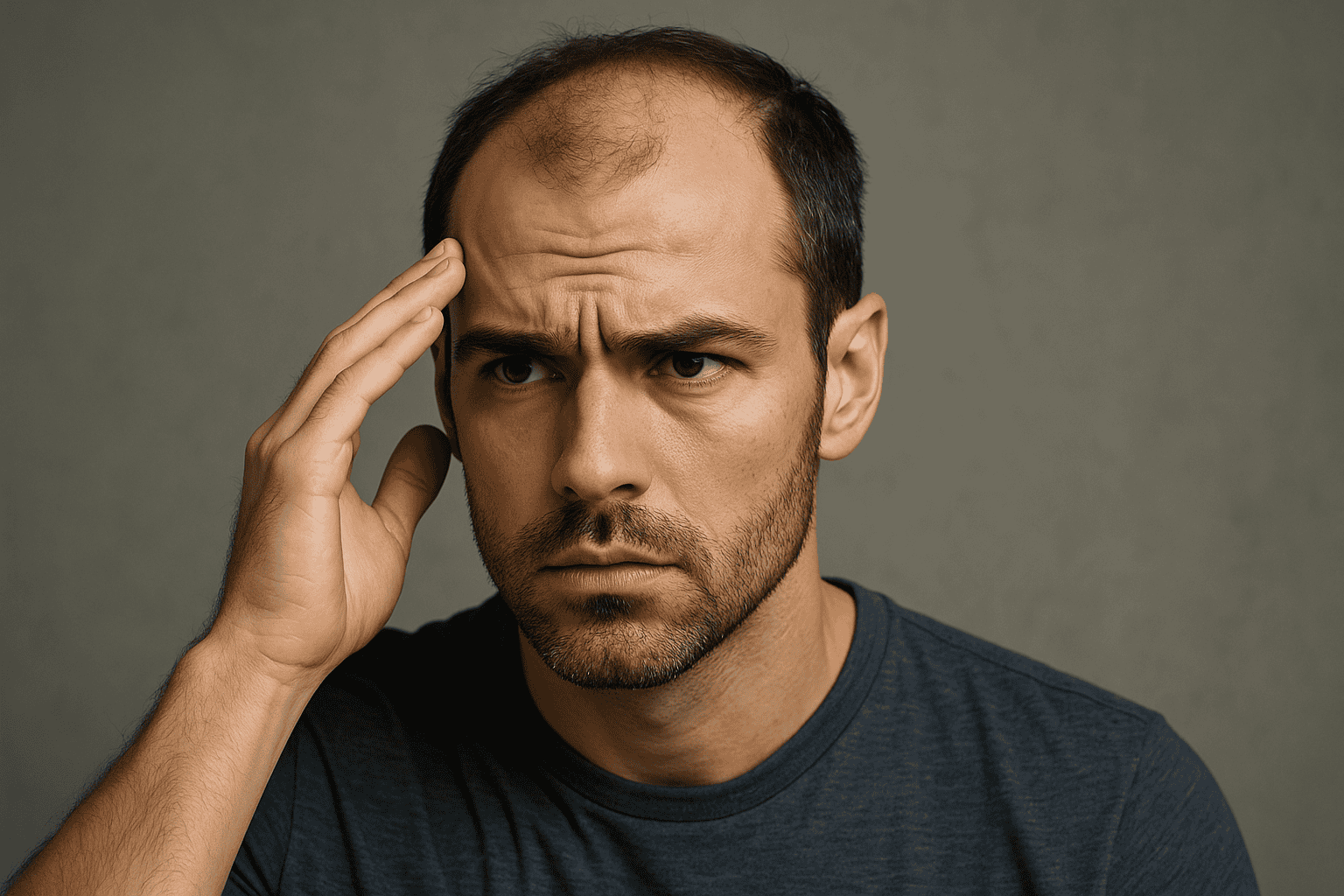
Hair transplantation is often viewed as a golden ticket to restoring a full head of hair. But the truth is more nuanced: not everyone is a good candidate. For many, it is either inadvisable at the current time or requires alternative treatments first. Understanding why you may not be a good candidate for a hair transplant can save you disappointment, expense and risk.
Below we explore the main reasons someone may not be suited to a hair transplant — including medical, anatomical, psychological and lifestyle factors. We’ll also link to useful resources and help you identify when full evaluation is needed.
One of the most fundamental requirements for a hair transplant is a robust donor area — typically the back and sides of the scalp where follicles are resistant to hormone-related hair loss.
If your donor area has low density, poor hair quality or already shows thinning, you may not have enough healthy follicles to harvest without creating visible thinning in the donor zone. Some clinics call this a “donor supply problem”.
What to ask your surgeon:
How many grafts do I realistically have available in the donor zone?
Does your assessment show the donor area is stable (i.e., not thinning further)?
If donor supply is limited, are alternative treatments possible (PRP, medication, hair systems)?
Without good donor hair, the chances of an excellent cosmetic result are greatly reduced.
If your hair loss pattern is still evolving — for example you’re very young, just beginning to recede or experiencing sudden diffuse shedding — a transplant may be premature.
Why this matters: even after transplanting follicles, if native hair continues to fall out around them, the result can look patchy or unnatural. A transplant should ideally be done when hair loss has stabilised.
Key questions for you:
How long have you had hair loss?
Have you tried non-surgical treatments (like minoxidil or finasteride) and waited for a response?
Is the hair loss pattern predictable (male pattern, female pattern) or random/patchy?
Waiting or stabilising hair loss may be a better option rather than rushing into surgery.
Certain medical and scalp conditions may contraindicate a hair transplant — or at least require treatment before proceeding.
Active scalp infections (e.g., folliculitis, tinea capitis) or inflammatory diseases (psoriasis, lupus) that disturb scalp skin health.
Scarring alopecia (areas of scar tissue on the scalp) which reduce blood supply and follicle viability.
Uncontrolled chronic medical illnesses (diabetes, bleeding disorders, immune suppression) which may complicate healing and graft survival.
Recommendation: A full medical evaluation with your surgeon (and potentially a dermatologist) should cover your scalp condition, systemic health and healing capacity. If issues are active, resolve them before transplant.
Even with perfect donor hair and stable hair loss, if your expectations are unrealistic a transplant can lead to dissatisfaction. You must understand what is achievable and what is not.
Examples of unrealistic expectations:
Expecting full head of youth hair when donor hair is limited.
Believing the transplant creates completely new hair rather than redistributing existing hair.
Believing the procedure is entirely risk-free, zero downtime or instant perfect result.
Helpful questions:
What density realistically can be achieved with my donor hair?
What will my hairline look like after 12–18 months?
What are the limitations and what happens if more hair falls out later?
Your surgeon should provide photo-examples and set realistic goals — if they don’t, you might not be a good candidate at this time.
Age is a less obvious but important factor. While hair transplants can be done on various age groups, younger patients (late teens, early 20s) who still have unpredictable, progressive hair loss may be at risk of future appearance issues.
Similarly, patients who have just experienced major shedding (e.g., postpartum telogen effluvium) or are within 12–18 months of significant hair loss event may benefit from waiting.
What to consider:
Is your hair loss recent and still fluctuating?
Will you likely lose more hair in the future?
Should you try medical treatments first and postpone transplant until the situation is clearer?
Certain lifestyle habits and personal health behaviours affect healing and transplant success. If you smoke, have poor nutrition, or do not adhere to post-op instructions, your outcome may suffer.
Things to watch:
Smoking reduces blood flow and delays healing.
Poor overall health, obesity or unmanaged diseases reduce graft survival.
Alcohol abuse or medications affecting clotting may increase risk during surgery.
If you are unwilling or unable to optimise these factors prior to surgery, you may not be a good candidate — at least for now.
Surprisingly, psychology plays a large role. If you have body dysmorphic disorder (BDD) or unrealistic body image issues, a hair transplant may not lead to satisfaction — and may even worsen distress.
Also, if your motivation is purely to please someone else or resolve non-hair-related insecurities, you may need counselling first rather than surgery.
Ask yourself:
Am I doing this for me, with realistic expectations?
Can I accept moderate improvement rather than perfection?
Am I psychologically prepared for possible “less than perfect” result or future hair loss?
If you find you’ve hit one or more of the “not good candidate” criteria, don’t worry — it doesn’t mean hopeless. It means you should explore alternative hair-restoration options, perhaps first.
Alternatives include:
Medical treatments (minoxidil, finasteride)
PRP (platelet-rich-plasma)
Low-level laser therapy
Hair systems or micro-scalp-pigmentation
It may be that these non-surgical approaches are more appropriate until your situation stabilises, donor hair improves, or medical issues are addressed.
A hair transplant can offer life-changing results — but only if the timing is right, your donor supply is sufficient, your medical and scalp health are good, and your expectations are managed. If one or more of the factors above apply to you, it doesn’t mean you’ll never get a transplant — it simply means now might not be the right time for a hair transplant.
A thorough consultation with a trusted hair-restoration specialist remains the best first step. Together you can assess your candidacy, explore non-surgical alternatives, stabilise your situation and then decide when (or if) to proceed.
Sage Medical. “Who Are Not Good Candidates for a Hair Transplant? Understanding the Factors.” October 2024. Sage Medical
Dr Bonaros Clinic. “Common FUE Hair Transplant Contraindications.” 2025. drbonaros.com
International Society of Hair Restoration Surgery / PMC. “Hair Transplant Practice Guidelines.” 2021. PMC
Dr Cinik Hair Transplant. “Can Anyone Get a Hair Transplant? The Complete List of Contraindications.” 2024.
Pizarro Hair Restoration. “The 5 Common Disqualifying Factors for Hair Transplant.” 2025. Pizarro Hair Restoration Clinic
Pasadena Hair Transplant. “Who May Not Be a Good Candidate for a Hair Transplant?” 2023. Pasadena Hair Transplant
Summary