
Brazilian Butt Lift Surgery in Turkey: Procedure, Safety, and Cost Breakdown
The Brazilian Butt Lift (BBL) has become one of the most in-demand cosmetic procedures worldwide—and Turkey has emerged as one […]
Perineorrhaphy surgery has become an increasingly recommended procedure for women who experience postpartum perineal trauma, pelvic floor weakness, or discomfort […]

Perineorrhaphy surgery has become an increasingly recommended procedure for women who experience postpartum perineal trauma, pelvic floor weakness, or discomfort caused by structural changes in the perineal region. While the term may sound clinical, the goal of perineorrhaphy is very human: to restore function, comfort, and confidence.
Whether you’re a patient researching treatment options or a clinician providing pelvic health solutions, understanding who needs perineorrhaphy surgery and how it improves pelvic well-being is essential. This guide explores the procedure in a clear, practical, and medically accurate way.
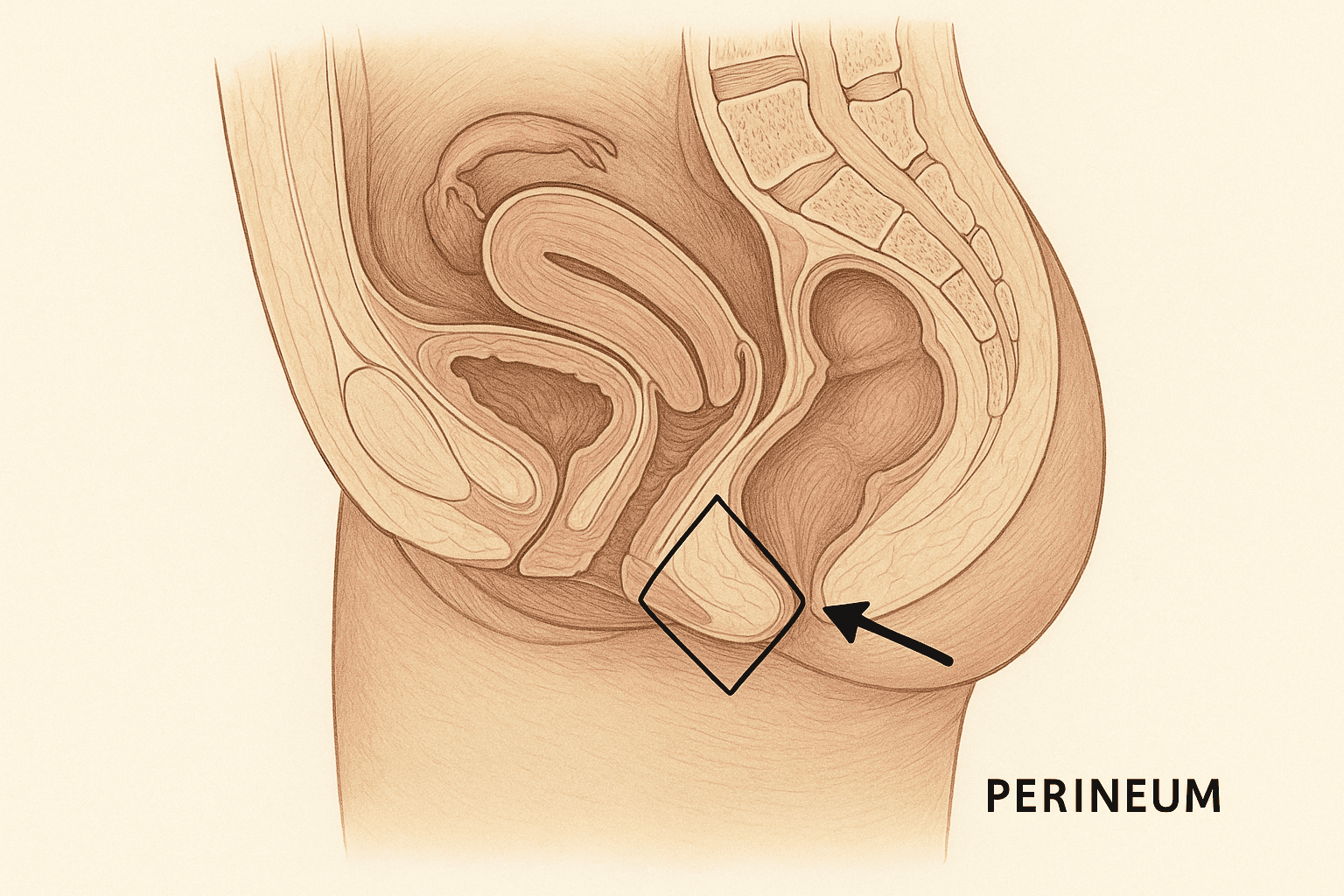
Perineorrhaphy is a surgical repair of the perineum—the area between the vagina and the anus. It is performed to reconstruct or strengthen tissues that have been:
Stretched
Torn
Scarred
Damaged during childbirth
Weakened due to aging or chronic strain
Unlike perineoplasty (which focuses mostly on cosmetic refinement), perineorrhaphy is primarily functional, targeting:
Pelvic floor support
Vaginal opening stability
Perineal muscle integrity
Symptom relief
The result is better pelvic function, reduced discomfort, and improved quality of life.
Perineorrhaphy is not limited to postpartum women. However, childbirth is the most common cause of perineal damage. You may be a candidate for perineorrhaphy surgery if you experience:
Natural childbirth—especially with:
Large babies
Instrumental delivery (forceps/vacuum)
Rapid labor
Episiotomy
—can lead to tears that do not fully heal.
Symptoms may include:
A widened vaginal opening
Persistent perineal discomfort
Difficulty during intercourse
Scar tissue sensitivity
Perineorrhaphy surgery restores anatomical support by repairing the torn muscles and fascia.
Weakness in pelvic floor muscles can lead to:
Vaginal laxity
A feeling of “openness”
Reduced sexual sensation
Mild pelvic organ prolapse
Difficulty retaining tampons
Perineorrhaphy improves structural support, enhancing pelvic strength and function.
Improper healing of perineal tissue can cause:
Pain
Burning
Tightness
Pinching sensations
Repairing scar tissue and restoring the perineum helps reduce discomfort.
Some women experience:
Air entrapment (“vaginal wind”)
A visible gap in the perineal area
Reduced support during physical activity
Perineorrhaphy tightens and reconstructs the area for better stability.
In some cases, scar tissue heals poorly, creating:
Lumps
Irregular tissue
Pain on pressure
Cosmetic dissatisfaction
Surgical revision smooths and rebuilds the tissue.
Hormonal shifts and tissue thinning can contribute to perineal laxity even without childbirth. Perineorrhaphy can restore comfort and improve pelvic integrity.
Perineorrhaphy is far more than a cosmetic tightening procedure. Its benefits are functional, anatomical, and psychological.
Strengthening the perineal body improves the foundation of the pelvic floor. This results in:
Better bladder support
Improved bowel control
Reduced risk of prolapse progression
It helps women regain stability they may have lost after childbirth or aging.
Many women experience increased satisfaction after perineorrhaphy due to:
Improved muscle tone
Restored vaginal opening control
Reduced pain during intercourse
Elimination of scar sensitivity
Reconstruction directly affects both comfort and confidence.
By tightening the perineal opening and rebuilding the supporting muscles, the surgery helps:
Reduce unwanted air entry
Improve sensation
Restore a more natural shape
This directly improves pelvic dynamics.
Removing problematic scar tissue and correcting asymmetry can significantly reduce daily discomfort, especially during sitting, exercise, or sex.
Women often report:
Increased confidence
No more embarrassment during exercise
Better sexual well-being
Ability to resume physical activities comfortably
A feeling of being “put back together” after childbirth
For many, perineorrhaphy is restorative both physically and emotionally.
The procedure typically lasts 30–60 minutes and may be performed under:
Local anesthesia
Regional anesthesia
General anesthesia (less common)
Removing or revising scar tissue
Re-approximating perineal muscles
Tightening the vaginal opening
Supporting the pelvic floor fascia
Closing the area with absorbable sutures
Most patients go home the same day.
Recovery is generally smooth with proper care.
Mild swelling for 1–2 weeks
Temporary discomfort (manageable with medication)
Return to light activities within a few days
Avoid intercourse and strenuous exercise for 6–8 weeks
Full healing usually occurs in 6–12 weeks.
Many women report significant improvement in symptoms within the first month.
If you’re considering perineorrhaphy, consulting a specialist in pelvic floor and postpartum reconstruction is essential. You can explore experienced obstetricians and gynecologists on Tabeebo’s directory.
No. Perineorrhaphy is primarily functional, focusing on repairing and strengthening the perineal muscles and supporting tissues. Perineoplasty is more cosmetic, aimed at improving the appearance of the vaginal opening and perineum.
Most women return to light activities within a few days. Full healing takes 6–12 weeks, and sexual intercourse should be avoided for at least 6–8 weeks.
Yes. By repairing torn muscles, reducing laxity, and eliminating scar pain, perineorrhaphy often enhances sexual comfort and sensation.
Perineorrhaphy helps support the pelvic floor, but it does not fully correct moderate or severe pelvic organ prolapse. Additional pelvic floor surgery may be needed depending on the severity.
No. While childbirth is the most common cause of perineal damage, aging, hormonal changes, or trauma may also lead someone to need perineorrhaphy.
Risks are minimal but may include:
Temporary swelling or discomfort
Infection (rare)
Painful scar tissue (preventable with proper technique and care)
Over-tightening (correctable)
Choosing an experienced gynecologic surgeon reduces complication risks significantly.
Abdool Z, Thakar R, Sultan AH. “Postpartum perineal muscles: clinical relevance and management.” International Urogynecology Journal.
American Urogynecologic Society (AUGS). “Pelvic floor dysfunction and reconstructive surgery recommendations.”
Cleveland Clinic. “Perineorrhaphy and pelvic floor repair information.”
Journal of Obstetrics and Gynecology Research. Studies on perineal repair outcomes.
Summary