
“Chronic Pain with No Cause? The Hidden Impact of Psychosomatic Disorders”
Ever experienced a mysterious pain that left doctors scratching their heads? You’ve been through a battery of tests, and everything […]
Autoimmune diseases occur when the body’s immune system mistakenly attacks its own tissues. These conditions can affect various parts of […]
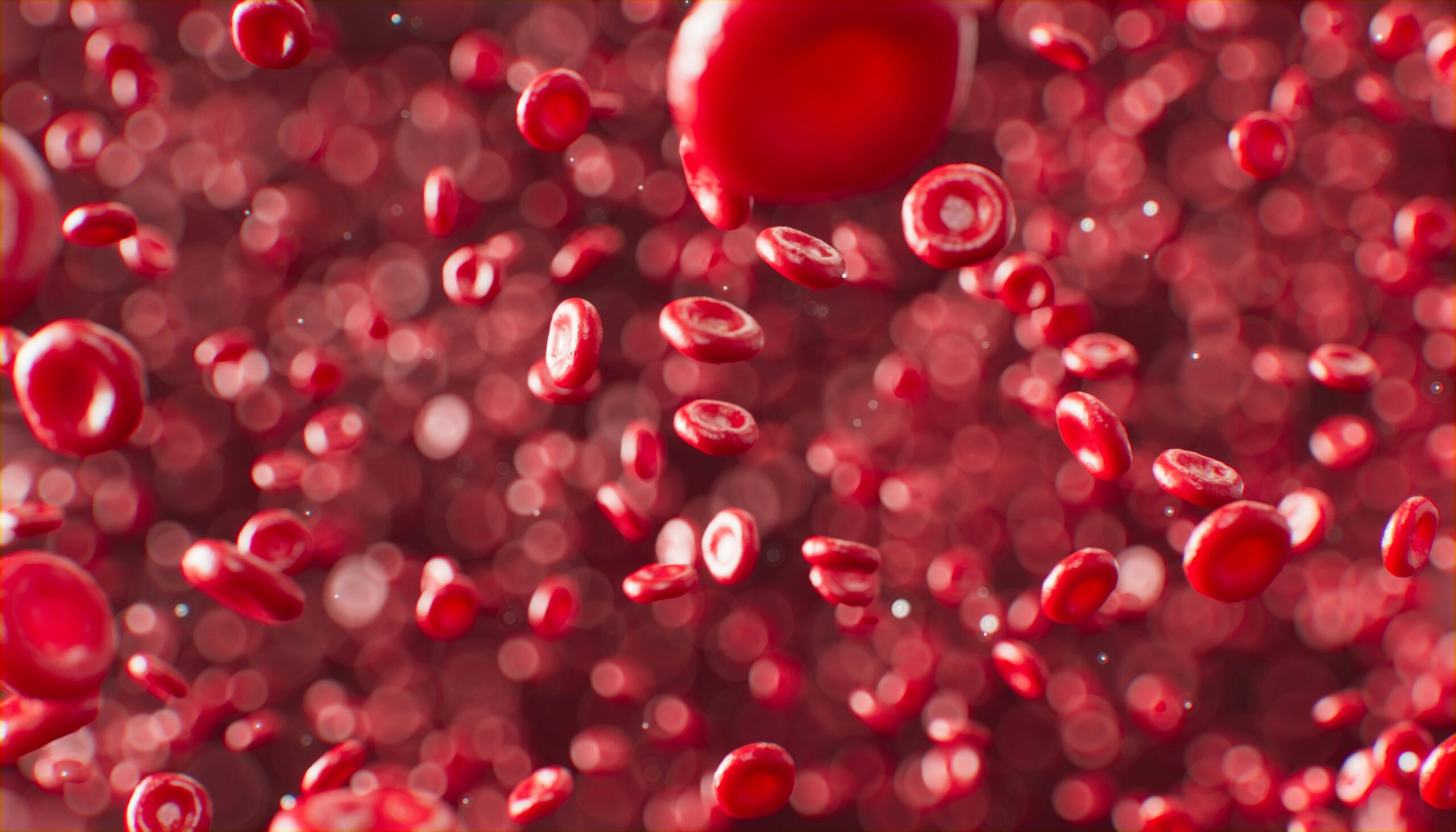
Autoimmune diseases occur when the body’s immune system mistakenly attacks its own tissues. These conditions can affect various parts of the body and lead to a range of symptoms and complications. There are more than 100 known autoimmune diseases, each with its unique characteristics. This comprehensive guide covers the most common types, causes, treatments, and management strategies, providing valuable insights into these complex conditions.
There are over 100 autoimmune diseases, but here are some of the most common ones:
1. Rheumatoid Arthritis (RA)
Rheumatoid arthritis is a chronic inflammatory disorder that primarily affects the joints. It causes pain, swelling, and stiffness, and can lead to joint damage and deformities.
2. Systemic Lupus Erythematosus (SLE)
SLE, commonly known as lupus, is a systemic condition that can affect the skin, joints, kidneys, brain, and other organs. Symptoms vary widely but often include fatigue, joint pain, and a butterfly-shaped rash on the face.
3. Multiple Sclerosis (MS)
Multiple sclerosis affects the central nervous system, disrupting the communication between the brain and the rest of the body. Symptoms include numbness, weakness, balance issues, and cognitive changes.
4. Type 1 Diabetes
Type 1 diabetes occurs when the immune system attacks insulin-producing cells in the pancreas. This leads to high blood sugar levels and requires lifelong insulin therapy.
5. Hashimoto’s Thyroiditis
Hashimoto’s thyroiditis is an autoimmune disorder affecting the thyroid gland, leading to hypothyroidism. Symptoms include fatigue, weight gain, and sensitivity to cold.
6. Psoriasis
Psoriasis is a skin condition where the immune system causes skin cells to multiply rapidly, leading to thick, red, scaly patches. It often affects the elbows, knees, and scalp.
7. Inflammatory Bowel Disease (IBD)
IBD encompasses conditions like Crohn’s disease and ulcerative colitis, where the immune system attacks the gastrointestinal tract, causing inflammation, pain, and digestive issues.
8. Graves’ Disease
Graves’ disease affects the thyroid, causing hyperthyroidism. Symptoms include anxiety, hand tremors, heat sensitivity, weight loss, and bulging eyes.
9. Celiac Disease
Celiac disease is triggered by the ingestion of gluten, leading to damage in the small intestine. Symptoms include diarrhea, bloating, gas, and malnutrition.
10. Sjogren’s Syndrome
Sjogren’s syndrome affects moisture-producing glands, leading to dry eyes and mouth. It can also affect other parts of the body, including joints and skin.
The exact causes of autoimmune diseases are not fully understood, but several factors are believed to contribute:
1. Genetic Factors
A family history of autoimmune diseases increases the risk, suggesting a genetic predisposition.
2. Environmental Triggers
Infections, exposure to certain chemicals, and other environmental factors can trigger autoimmune responses in genetically susceptible individuals.
3. Hormonal Influences
Hormones play a role, as autoimmune diseases are more common in women, particularly during reproductive years.
4. Immune System Dysregulation
Defects in the immune system can lead to a failure in distinguishing between self and non-self, causing it to attack the body’s own tissues.
5. Stress
Chronic stress can exacerbate symptoms and trigger flare-ups. Stress management techniques can help reduce the impact of stress on autoimmune diseases.
Autoimmune diseases vary widely in their severity and impact. While some can be life-threatening, most are chronic and lifelong conditions that require ongoing management. With proper treatment and lifestyle adjustments, many people with autoimmune diseases can lead full and active lives.
a. Anti-Inflammatory Drugs
Nonsteroidal anti-inflammatory drugs (NSAIDs) and corticosteroids help reduce inflammation and relieve pain. Examples include ibuprofen (Advil) and prednisone.
b. Immunosuppressants
Medications like methotrexate and azathioprine suppress the immune system to prevent it from attacking healthy tissues.
c. Biologics
Biologic agents target specific components of the immune system. Examples include TNF inhibitors like infliximab (Remicade) and adalimumab (Humira) for RA and MS.
d. Disease-Modifying Antirheumatic Drugs (DMARDs)
DMARDs slow disease progression and prevent joint damage in conditions like RA. Examples include methotrexate and hydroxychloroquine.
a. Diet and Nutrition
A balanced diet rich in anti-inflammatory foods, such as fruits, vegetables, and omega-3 fatty acids, can help manage symptoms.
b. Exercise
Regular physical activity improves overall health, reduces inflammation, and maintains joint mobility.
c. Stress Management
Techniques like yoga, meditation, and mindfulness can reduce stress, which may exacerbate autoimmune symptoms.
a. Acupuncture
Acupuncture may help reduce pain and improve well-being in some patients with autoimmune diseases.
b. Herbal Supplements
Certain herbs and supplements, like turmeric and omega-3s, have anti-inflammatory properties and may support conventional treatments.
1. Regular Monitoring
Routine check-ups and blood tests are crucial for monitoring disease activity and adjusting treatments.
2. Patient Education
Understanding the disease, its triggers, and management strategies empowers patients to take an active role in their care.
3. Support Networks
Joining support groups and connecting with others facing similar challenges can provide emotional support and practical advice.
Autoimmune diseases can affect anyone, but certain factors influence the risk:
1. Personalized Medicine
Advances in genetic testing and biomarkers are paving the way for personalized treatment plans tailored to individual patients.
2. New Biologic Agents
Research continues to develop new biologic agents that target specific immune pathways with fewer side effects.
3. Gut Microbiome
Studies on the gut microbiome suggest that gut health plays a significant role in autoimmune diseases, leading to new potential therapies.
4. Stem Cell Therapy
Stem cell research holds promise for regenerating damaged tissues and modulating the immune system to treat autoimmune diseases.
1. What are common symptoms of autoimmune diseases?
Symptoms vary but often include fatigue, joint pain, swelling, skin rashes, and gastrointestinal issues.
2. Can autoimmune diseases be cured?
There is currently no cure, but treatments can effectively manage symptoms and improve quality of life.
3. Are autoimmune diseases hereditary?
There is a genetic component, so having a family member with an autoimmune disease increases the risk.
4. How are autoimmune diseases diagnosed?
Diagnosis involves blood tests, imaging studies, and a thorough clinical evaluation by a healthcare provider.
5. What is the role of diet in managing autoimmune diseases?
A healthy diet can help reduce inflammation and manage symptoms. Specific dietary recommendations vary depending on the disease.
6. Can stress trigger autoimmune diseases?
Chronic stress can exacerbate symptoms and trigger flare-ups in some individuals. Stress management is an important part of treatment.
7. What is the difference between autoimmune diseases and allergies?
Autoimmune diseases involve the immune system attacking the body’s own tissues, while allergies involve an overreaction to external substances like pollen or food.
8. Is there a link between autoimmune diseases and cancer?
Some autoimmune diseases can increase the risk of certain cancers due to chronic inflammation and immune system dysregulation.
9. What role does exercise play in managing autoimmune diseases?
Regular exercise can reduce inflammation, improve mood, and maintain joint function, helping manage symptoms.
10. How important is early diagnosis and treatment?
Early diagnosis and treatment are crucial for preventing severe complications and improving long-term outcomes.
Autoimmune diseases are complex conditions that require a multifaceted approach to diagnosis, treatment, and management. Understanding the types, causes, and available treatments can help patients and caregivers navigate these challenges more effectively. With ongoing research and advancements, the future holds promise for more personalized and effective therapies, improving the quality of life for those affected by autoimmune diseases.
Summary